Meniscal injuries are among the most common and debilitating knee conditions, especially affecting athletes and active adults. Conventional treatments such as suturing and partial meniscectomy often fail to restore full knee function, sometimes even accelerating joint degeneration and leading to osteoarthritis. Addressing these critical limitations, researchers have introduced an innovative solution: a tunable extracellular matrix (ECM)-based hydrogel system designed for precise, zone-specific meniscal repair.
Why Meniscus Zonal Specificity Matters
The meniscus, a crescent-shaped cartilage cushioning the knee joint, comprises three distinct zones:
- Outer Zone (Red-Red): Richly vascularized, containing robust type-I collagen, facilitating strong natural healing capabilities.
- Intermediate Zone (Red-White): Moderately vascularized with intermediate healing potential.
- Inner Zone (White-White): Avascular, severely limiting healing potential and presenting significant repair challenges (Lee et al., 2025).
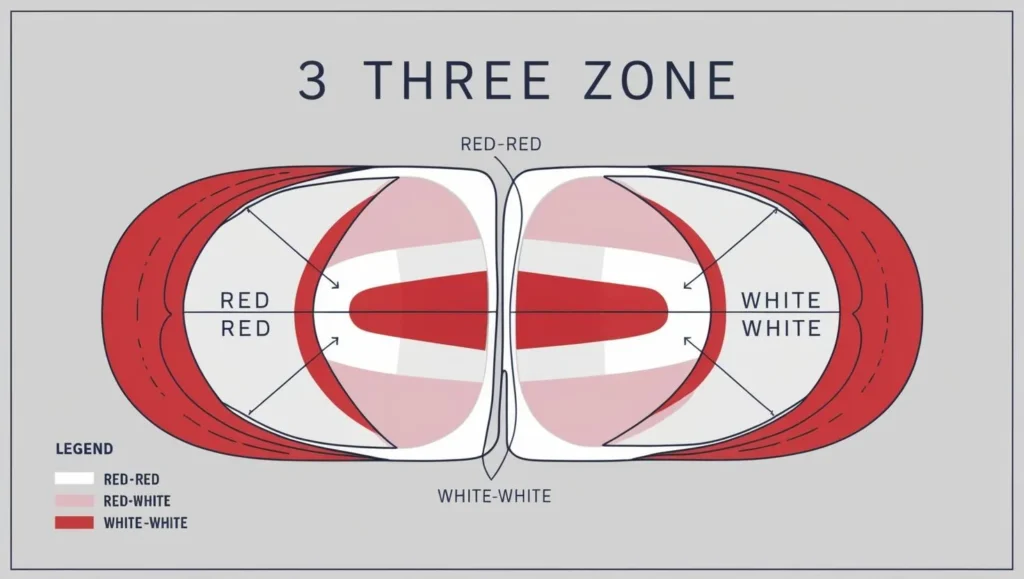
Each zone’s cellular composition and mechanical properties differ significantly, influencing healing capabilities and necessitating customized treatment strategies.
Common Meniscal Tears and Current Limitations
Meniscal tears typically occur as:
- Longitudinal Tears: Parallel to the meniscal edge, common among young athletes.
- Radial Tears: Extend across the meniscus, critically disrupting load-bearing functions.
- Horizontal Tears: Usually degenerative, occurring within meniscal layers (AAOS).
Traditional repair methods struggle, particularly with complex tear patterns. Suturing is primarily effective for simpler, outer-zone tears but often fails in complex or inner-zone cases. Arthroscopic Partial Meniscectomy (APM), while temporarily relieving symptoms, significantly increases osteoarthritis risk (Journal of Orthopaedic Surgery and Research).
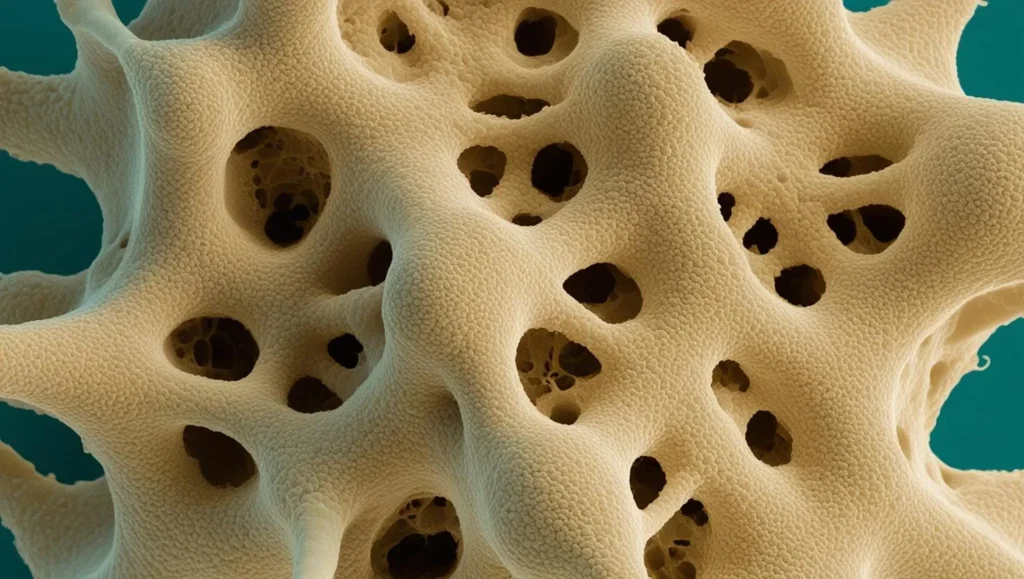
Introducing Decellularized Extracellular Matrix (DEM) Hydrogels
DEM hydrogels are regenerative biomaterials derived from natural tissues, capable of supporting cellular growth, adhesion, and differentiation. However, conventional DEM hydrogels lack sufficient zonal specificity. Researchers have developed advanced, tunable ECM-based hydrogels derived from fetal (FDEM) and adult (ADEM) bovine ECM to mimic meniscal zonal heterogeneity effectively (Lee et al., 2025).
Tunable ECM-Based Hydrogels: Innovative Solutions
The advanced hydrogel system combines fetal and adult ECM, tailoring their biochemical and mechanical properties:
- Fetal ECM (FDEM): Softer, promoting chondrogenic tissue regeneration, ideal for inner-zone repairs.
- Adult ECM (ADEM): Stiffer, encouraging fibrochondrogenic responses suited for outer-zone injuries.
A hybrid form (FADEM) precisely adjusts hydrogel properties to the unique needs of each meniscal zone.
How ECM Composition Influences Cellular Behavior
The ECM’s composition significantly influences essential cellular behaviors:
- Cell Shape Adaptation: ECM stiffness influences cell morphology and subsequent tissue regeneration.
- Mechanical Signaling: Regulates critical pathways like YAP nuclear localization, guiding tissue-specific cell differentiation.
- Gene Expression: Activates either fibrochondrogenic or chondrogenic pathways, depending on targeted zones.
Proteomic analyses highlight essential proteins like fibronectin (exclusive to ADEM) and critical collagen and proteoglycans, supporting precise zonal regeneration (NIH Protein Database).
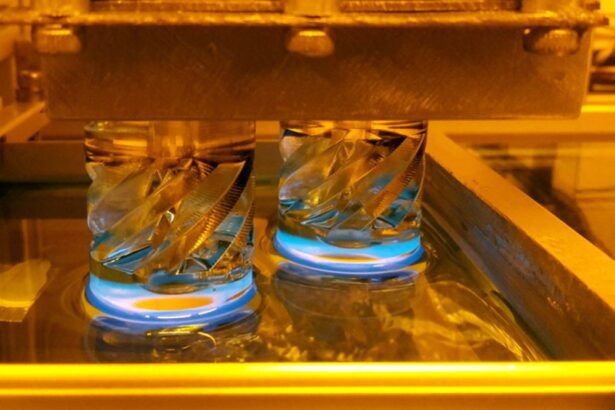
Enhancing Hydrogel Performance with Methacrylated Hyaluronic Acid (MeHA)
Integration of Methacrylated Hyaluronic Acid (MeHA) significantly enhances hydrogel performance:
- Adjustable Stiffness: Precisely matches zonal mechanical requirements.
- Improved Injectability: Facilitates minimally invasive delivery to injury sites.
- Supports 3D Bioprinting: Enables the creation of complex, tailored structures ideal for intricate meniscal injuries (Biomaterials Journal).
Proven Success in Animal and Ex Vivo Studies
Extensive testing validates the hydrogels’ exceptional biocompatibility, effective cellular recruitment, migration, and ECM deposition, ensuring robust, long-term regeneration and readiness for clinical applications (Lee et al., 2025).
Practical Applications: Customized Meniscal Repair Strategies
ECM-based hydrogels provide highly tailored solutions:
- Injectable Hydrogels: Perfect for targeted zone-specific or simpler tear repairs.
- Advanced 3D Bioprinting: Suitable for complex gradient-based biomaterial constructs tailored to specific injuries, promising improved patient outcomes and joint longevity.
Future Directions and Clinical Translation
Ongoing developments include:
- Enhanced replication of human ECM structures.
- Transition towards human-derived ECM.
- Comprehensive testing in larger animal models.
- Potential integration with cell-based therapies and growth factors for superior regenerative results (FDA Guidelines).
Conclusion: A Transformative Advance in Meniscal Repair
Tunable ECM-based hydrogels significantly advance meniscal repair strategies, overcoming the limitations of traditional methods by accurately replicating meniscal tissue’s unique zonal properties. This innovative approach holds considerable potential to enhance patient outcomes, making it a cornerstone of future regenerative medicine and tissue engineering.
References
- Lee, S.-H., Li, Z., Zhang, E.Y., et al. (2025). Precision repair of zone-specific meniscal injuries using a tunable extracellular matrix-based hydrogel system. Bioactive Materials. https://doi.org/10.1016/j.bioactmat.2025.02.013
- American Academy of Orthopaedic Surgeons (AAOS). Meniscal Tears. https://www.aaos.org/
- Biomaterials Journal. https://www.sciencedirect.com/journal/biomaterials
- FDA Guidelines for Regenerative Medicine. https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products
- NIH Protein Database. https://www.ncbi.nlm.nih.gov/protein